[ad_1]
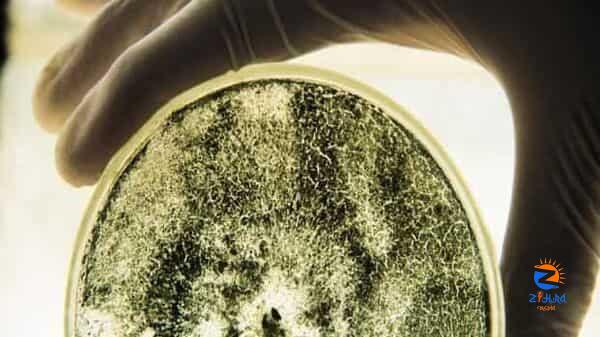
Candida auris, a fungus discovered about 15 years ago in Japan, infected at least 2,377 people in the U.S. in 2022, up from 53 in 2016, the Centers for Disease Control and Prevention said. Its swift spread into most states and more than 40 countries has prompted the CDC and World Health Organization to label it a growing threat to public health. Candida auris has a mortality rate of up to 60% and is particularly risky for people who are older or have compromised immune systems, the CDC said.
“To see a new species arrive on the scene and then suddenly emerge as a global pathogen less than 15 years later—that’s really remarkable,” said Dr. Peter Pappas, an infectious-disease specialist at the University of Alabama at Birmingham.
The first documented Candida auris infection in the U.S. was in 2013, CDC researchers said in a study published Monday in the Annals of Internal Medicine. The fungus has since expanded its range from centers of spread around New York City and Chicago to at least 28 states and Washington, D.C., the study said.
“Seeing the number of cases was alarming,” said Dr. Meghan Lyman, a CDC epidemiologist and lead author of the paper.
Most Candida auris transmission has occurred in healthcare facilities that provide long-term care to very sick patients, the paper said. Select Specialty Hospital-Northwest Detroit, a rehabilitation center for the critically ill, temporarily stopped admitting patients last year after an outbreak of Candida auris. All healthcare facilities need to be aware of the threat, said Buddy Hammerman, chief medical officer of Select Medical Holdings Corp., the hospital’s operator.
“Patients are becoming colonized with this organism and it’s becoming smarter than we are,” Dr. Hammerman said.
Candida auris is a yeast of mysterious origins. It was identified in 2009 after it was discovered in the ear of a patient in Japan. Microbiologists have scoured genomic databases and natural environments for clues into its origins and evolution. Outside of people, it has only been detected in two sites: a salt marsh and a sandy beach in the Andaman Islands, a remote archipelago in the Indian Ocean.
Candida auris might have lived in the environment or animals for a long time before a change spurred its spread in people, infectious-disease experts said. Rising global temperatures might have encouraged Candida auris to evolve more tolerance to heat, making it more adept at infecting people, whose body temperatures have long served as an effective barrier against invasive fungal disease, they said. Widespread use of disinfectants and antifungals on crops might have allowed Candida auris to thrive by killing off microbial competitors, they said.
Common disinfectants including bleach and alcohol aren’t always effective against Candida auris, which can colonize a person’s skin, said Andrej Spec, an associate professor of medicine at Washington University School of Medicine in St. Louis. Deep cleaning and special disinfectants that destroy spores are needed to limit its spread, he said.
“If someone is found to have Candida auris on their skin, you need to isolate them to try to prevent new people from being colonized,” Dr. Spec said.
Not everyone who encounters Candida auris is sickened, but if it infects the bloodstream, wounds or organs, the effects can be severe. The most common symptoms of Candida infection are fever and chills, the CDC said.
Fungal infections are estimated to kill at least 1.6 million people a year, according to Global Action for Fungal Infections, a research and fundraising nonprofit.
There are only three classes of antifungal drugs commonly used for severe fungal disease, Dr. Spec said, all of which can cause toxic side effects. Fungi are also developing resistance to these drugs, Dr. Spec said. At least seven Candida auris infections were resistant to available antifungals in 2021, the CDC said, up from four in the years before 2020.
Scynexis Inc. and Pfizer Inc. are developing drugs that have been shown in clinical trials to be effective against Candida auris. Cidara Therapeutics Inc. said it has submitted its drug rezafungin to the Food and Drug Administration for approval to treat Candida infections, including Candida auris. Rezafungin would be the first new drug for the treatment of invasive Candida infections in over a decade, the company said.
[ad_2]